Link to article on Pain Medicine News
Encouraging Results for Minimally Invasive Treatment for Lumbar Spinal Stenosis
To restore quality of life, to increase function, and to regain wholeness for patients suffering from chronic pain.
Monday, November 29, 2010
FDA approves Botox as migraine preventive
Helpful news for patients suffering from daily migraines 15 days or more in a month that last 4 hours or more! Botox -- Orginally known for smoothing out wrinkles on the face -- has been approved by the FDA to treat chronic migraines in adults. Call us to see how we can help migraine sufferers and work with your insurance to see if the procedure is covered. 512 219 8787
(CNN) -- Federal health authorities on Friday approved Botox injections for the prevention of chronic migraines in adults, an advance experts described as "modest."
In a statement, the Food and Drug Administration recommended Botox be injected approximately every three months around the head and neck to dull future headache symptoms.
The drug -- whose generic name is onabotulinumtoxinA -- has not been shown to work against migraines that occur 14 days or fewer per month, nor has it been shown to work for other forms of headache, said the statement.
Experiencing a migraine on most days "is one of the most disabling forms of headache," said Dr. Russell Katz, of the Division of Neurology Products in the FDA's Center for Drug Evaluation and Research. "This condition can greatly affect family, work, and social life, so it is important to have a variety of effective treatment options available."
Migraines, an intense pulsing or throbbing pain in one area of the head, are often accompanied by nausea, vomiting and sensitivity to light and sound, doctors say. Chronic migraines are defined as those that occur on 15 days or more for more than four hours per day.
The drug, made by Allergan, Inc., of Irvine, California, was approved last month in Britain for the same purpose.
The two company-funded studies submitted to the FDA involved 1,384 adults from 122 study sites in Europe and North America. They found that after six months, patients who got the drug experienced 7.8 and 9.2 fewer days of migraine than they had before the studies started. Those who got injections of placebo (sugar pill) experienced 6.4 and 6.9 fewer headache days.
Over those six months, patients on the drug experienced 107 and 134 fewer hours of headache, versus a reduction of 70 and 95 hours for those on placebo, according to the studies.
"The benefits are modest when you look at the overall results," said Dr. Elizabeth W. Loder, associate professor of neurology at Harvard Medical School and the chief of the division of headaches in the Department of Neurology at the Brigham and Women's Hospital in Boston. Loder was involved in an Allergan-funded trial several years ago but has no current relationship with the company.
"But, of course, within those results, there are always patients who do much better than the average and there are patients who don't have any benefit," she said.
Still, she added, "It will provide more options for patients who currently have very few forms of treatment available to them ... when you are dealing with a problem like this, even modest improvement can mean the difference between being able to go to work and not being able to function very well."
Dr. Joel Saper, director of the Michigan Head Pain and Neurological Institute and clinical professor of neurology at Michigan State University, said he has been using the drug for that purpose for more than a decade, even though it was not approved for it.
The FDA's approval will likely mean that insurance companies will pick up the tab for it now, he said. Saper, who has also participated in Allergan-funded trials, predicted "certain subsets of people will get dramatic results."
The most common adverse reactions reported by chronic migraine patients being treated with Botox were neck pain and headache, the FDA said.
About 1 percent of patients on the drug (versus 0.3 percent of those on placebo) found that their migraines worsened so much they had to be hospitalized, but it was generally well-tolerated, the company said.
In each study, less than 2 percent of patients dropped out of the study due to an adverse event.
The drug labeling warns that the effects of the botulinum toxin may spread beyond where it is injected, causing symptoms that may include life-threatening difficulties swallowing and breathing.
Botox is sold to doctors in 200-unit vials that cost $1,050, said Cyrstal Muilenburg, spokeswoman for Allergan. Last year, the drug had sales of $1.3 billion, she said.
Doctors gave administered a total of 155 units to each migraine patient in 31 injections into muscles of the head and neck, she said. The treatment was repeated at three-month intervals.
Some 3.2 million Americans are estimated to suffer from chronic migraine, though some 80 percent of them have never been diagnosed as having the disease, the company said.
The World Health Organization ranks migraine as the 19th most disabling disease. Women are three times as likely as men to suffer from migraines, which are also linked to depression and anxiety.
The drug is the same chemical entity that was approved 21 years ago for the treatment of strabismus and blepharospasm, two eye-muscle disorders.
Since then, regulators in some 80 countries have approved it for 21 different indications, including treatment of the abnormal head position and neck pain associated with cervical dystonia in adults, symptoms of severe underarm sweatingand treatment of increased muscle stiffness in elbow, wrist and finger muscles in adults with upper-limb spasticity.
By Tom Watkins, CNN
(CNN) -- Federal health authorities on Friday approved Botox injections for the prevention of chronic migraines in adults, an advance experts described as "modest."
In a statement, the Food and Drug Administration recommended Botox be injected approximately every three months around the head and neck to dull future headache symptoms.
The drug -- whose generic name is onabotulinumtoxinA -- has not been shown to work against migraines that occur 14 days or fewer per month, nor has it been shown to work for other forms of headache, said the statement.
Experiencing a migraine on most days "is one of the most disabling forms of headache," said Dr. Russell Katz, of the Division of Neurology Products in the FDA's Center for Drug Evaluation and Research. "This condition can greatly affect family, work, and social life, so it is important to have a variety of effective treatment options available."
Migraines, an intense pulsing or throbbing pain in one area of the head, are often accompanied by nausea, vomiting and sensitivity to light and sound, doctors say. Chronic migraines are defined as those that occur on 15 days or more for more than four hours per day.
The drug, made by Allergan, Inc., of Irvine, California, was approved last month in Britain for the same purpose.
The two company-funded studies submitted to the FDA involved 1,384 adults from 122 study sites in Europe and North America. They found that after six months, patients who got the drug experienced 7.8 and 9.2 fewer days of migraine than they had before the studies started. Those who got injections of placebo (sugar pill) experienced 6.4 and 6.9 fewer headache days.
Over those six months, patients on the drug experienced 107 and 134 fewer hours of headache, versus a reduction of 70 and 95 hours for those on placebo, according to the studies.
"The benefits are modest when you look at the overall results," said Dr. Elizabeth W. Loder, associate professor of neurology at Harvard Medical School and the chief of the division of headaches in the Department of Neurology at the Brigham and Women's Hospital in Boston. Loder was involved in an Allergan-funded trial several years ago but has no current relationship with the company.
"But, of course, within those results, there are always patients who do much better than the average and there are patients who don't have any benefit," she said.
Still, she added, "It will provide more options for patients who currently have very few forms of treatment available to them ... when you are dealing with a problem like this, even modest improvement can mean the difference between being able to go to work and not being able to function very well."
Dr. Joel Saper, director of the Michigan Head Pain and Neurological Institute and clinical professor of neurology at Michigan State University, said he has been using the drug for that purpose for more than a decade, even though it was not approved for it.
The FDA's approval will likely mean that insurance companies will pick up the tab for it now, he said. Saper, who has also participated in Allergan-funded trials, predicted "certain subsets of people will get dramatic results."
The most common adverse reactions reported by chronic migraine patients being treated with Botox were neck pain and headache, the FDA said.
About 1 percent of patients on the drug (versus 0.3 percent of those on placebo) found that their migraines worsened so much they had to be hospitalized, but it was generally well-tolerated, the company said.
In each study, less than 2 percent of patients dropped out of the study due to an adverse event.
The drug labeling warns that the effects of the botulinum toxin may spread beyond where it is injected, causing symptoms that may include life-threatening difficulties swallowing and breathing.
Botox is sold to doctors in 200-unit vials that cost $1,050, said Cyrstal Muilenburg, spokeswoman for Allergan. Last year, the drug had sales of $1.3 billion, she said.
Doctors gave administered a total of 155 units to each migraine patient in 31 injections into muscles of the head and neck, she said. The treatment was repeated at three-month intervals.
Some 3.2 million Americans are estimated to suffer from chronic migraine, though some 80 percent of them have never been diagnosed as having the disease, the company said.
The World Health Organization ranks migraine as the 19th most disabling disease. Women are three times as likely as men to suffer from migraines, which are also linked to depression and anxiety.
The drug is the same chemical entity that was approved 21 years ago for the treatment of strabismus and blepharospasm, two eye-muscle disorders.
Since then, regulators in some 80 countries have approved it for 21 different indications, including treatment of the abnormal head position and neck pain associated with cervical dystonia in adults, symptoms of severe underarm sweatingand treatment of increased muscle stiffness in elbow, wrist and finger muscles in adults with upper-limb spasticity.
Wednesday, November 24, 2010
Happy Thanksgiving
We have so much to be thankful for this season.
Republic Spine and Pain would like to wish Austin, Cedar Park, Leander, Lago Vista and Round Rock a wonderful holiday with your loved ones.
Best wishes in health and happiness,
Dr Yeh, Dr Ostadian, Jamika, Maria & Mona
Republic Spine and Pain would like to wish Austin, Cedar Park, Leander, Lago Vista and Round Rock a wonderful holiday with your loved ones.
Best wishes in health and happiness,
Dr Yeh, Dr Ostadian, Jamika, Maria & Mona
Monday, November 22, 2010
FDA pulls common pain med off the market
Important Pain Managament News - If you are a patient at Republic Spine and Pain and have questions about the Pain Medications you are currently taking please call our staff at Republic Pain. Making sure Austin Pain Management patients are well informed about their medications is important to us.
By the CNN Wire Staff
By the CNN Wire Staff
November 19, 2010 2:40 p.m. EST
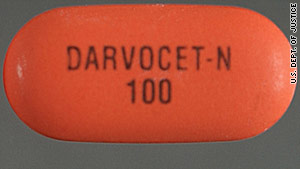
Washington (CNN) -- The pharmaceutical company that makes the prescription pain medications Darvon and Darvocet has agreed to withdraw the drugs from the U.S. market at the request of the U.S. Food and Drug Administration, the FDA said Friday.
"We recommend to physicians stop prescribing the drugs. As for patients, do not stop taking it, but we urge you to contact your health care professional. Do not delay," said Gerald Dal Pan, director of the FDA's Office of Surveillance and Epidemiology.
Xanodyne Pharmaceuticals Inc. manufactures Darvon and Darvocet, two brand name versions of propoxyphene. The FDA also asked generic makers of the pain medicine to voluntarily remove their products.
The decision to remove the drug came after the FDA reviewed a new trial study that looked at the drug's impact on heart rhythms.
"The drug's effectiveness in reducing pain is no longer enough to outweigh the drug's serious potential heart risks," the FDA said in a statement released Friday.
Propoxyphene, first approved by the FDA in 1957, is an opioid used to treat mild to moderate pain. It is sold under various names both alone, such as Darvon, or in combination with acetaminophen, such as Darvocet.Since 1978, the FDA has received two requests to remove propoxyphene from the market, but concluded that the benefits of propoxyphene for pain relief at recommended doses outweighed the safety risks.
Saturday, November 20, 2010
Could Losing Weight Help Arthritis Pain?
Our Pain Management physicians strongly believe that any treatment plan should be combined with exercise when possible. There are a great selection of parks, gyms, physical therapists in Austin to support your decision to get active.
WebMD Feature
WebMD Feature
By Gina Shaw
Reviewed By Brunilda Nazario, MD
For 12 years, Robin Lutchansky spent most of her time in a wheelchair. The pain from her severe osteoarthritis, first diagnosed in her early 30s, made it difficult to walk more than short distances.
Today, Lutchansky is out of the wheelchair and back at work as a public relations representative for a high-tech firm, and says that her daily pain levels have gone from an 8 or a 9 to a 1. “It’s amazing. It’s a new life. I had no idea it was possible.”
“When we walk, when we go up and down stairs, or get into or out of a chair or car, we can put three to five times our body weight, and sometimes more, on the joints,” says Geoffrey Westrich, attending orthopedic surgeon and Director of Joint Replacement Research at the Hospital for Special Surgery in New York. “So if you’re 50 pounds overweight, you’re putting around 250 pounds of increased stress across your knees and hips.”
Over time, that extra weight makes you much more prone to developing arthritis and can cause arthritis to progress much more rapidly, leading to much more pain once it has developed.
Fortunately, the same principle works in reverse. “For every pound people lose, they lose 3 pounds of stress across their knee and 6 pounds of stress on their hip, on average,” says Westrich.
Jane Angelich, a 58-year-old California businesswoman, has lost 33 pounds on Weight Watchers.
“What a difference!” she says. “It starts when I get out of bed in the morning. No more limping around and groaning for the first few minutes. Instead of finding excuses to sit on my couch instead of walking around, I now walk the equivalent of a 5k without any issues and can even function the next day!”
High-impact exercise, like running, jogging, and aerobics, can put too much stress on the joints, so doctors recommend against these activities. “They can hasten the arthritis process and cause injury,” says Westrich.
Instead, Vangsness recommends that his patients pursue one of three types of exercise that are particularly well suited for people with arthritis:
He adds that some of his extremely obese patients have gotten their weight loss started through gastric bypass or gastric banding surgery. “They start peeling off the pounds, and this tremendous loss of weight really knocks down their pain,” he says. “It’s like a whole new knee. And after losing that weight, they can exercise where they couldn’t before, strengthen their muscles, and further reduce pain.”
Then, a little over three years ago, Lutchansky found her way to a pain management clinic that taught her how to exercise -- first, teaching her how to walk again. Over the next three years, Lutchansky, now 51, gradually lost nearly 100 pounds with calorie reduction and exercise.
“I did it slowly. I started out just lifting 2-pound weights, and I walked in the pool every day,” she says.Today, Lutchansky is out of the wheelchair and back at work as a public relations representative for a high-tech firm, and says that her daily pain levels have gone from an 8 or a 9 to a 1. “It’s amazing. It’s a new life. I had no idea it was possible.”
What Weight Does to Your Joints
If you are at all overweight, one of the best ways to reduce osteoarthritis pain is by taking off excess pounds. Being overweight increases the load that you put on your joints -- your knees, your hips, your ankle -- with every step you take.“When we walk, when we go up and down stairs, or get into or out of a chair or car, we can put three to five times our body weight, and sometimes more, on the joints,” says Geoffrey Westrich, attending orthopedic surgeon and Director of Joint Replacement Research at the Hospital for Special Surgery in New York. “So if you’re 50 pounds overweight, you’re putting around 250 pounds of increased stress across your knees and hips.”
Over time, that extra weight makes you much more prone to developing arthritis and can cause arthritis to progress much more rapidly, leading to much more pain once it has developed.
Fortunately, the same principle works in reverse. “For every pound people lose, they lose 3 pounds of stress across their knee and 6 pounds of stress on their hip, on average,” says Westrich.
Small Steps, Big Changes
You don’t have to lose 100 pounds, like Lutchansky, to see a difference in your pain levels. C. Thomas Vangsness, Jr., MD, professor of orthopaedic surgery and chief of sports medicine at the Keck School of Medicine at the University of Southern California, says most of his arthritis patients who lose weight notice that their pain is diminishing after losing about 20 pounds.Jane Angelich, a 58-year-old California businesswoman, has lost 33 pounds on Weight Watchers.
“What a difference!” she says. “It starts when I get out of bed in the morning. No more limping around and groaning for the first few minutes. Instead of finding excuses to sit on my couch instead of walking around, I now walk the equivalent of a 5k without any issues and can even function the next day!”
Small Steps, Big Changes continued...
Losing weight cannot repair the damage that’s already been done to your joints by arthritis, but in addition to decreasing your pain, it can also help to slow down the further progression of the disease. One study found that knee osteoarthritis in obese men would decrease by 21.5% if they lost enough weight to be categorized as merely overweight; for women, arthritis would decrease by 31%.
“The damage is already done, and arthritis is a progressive process,” says Westrich. “But weight loss can be tremendously helpful in alleviating pain, allowing greater function, and prolonging the period of time before someone needs joint replacement surgery.”
And if you haven’t developed arthritis but you’re worried about it, losing excess weight can significantly lower your risk. If you’re significantly overweight, every 11 pounds you lose cuts your risk of developing arthritis by more than 50%.Making It Happen
The best way to lose weight, any doctor will tell you, is to eat less, eat healthy foods, and exercise more. But while someone with arthritis can start to change their eating habits in pretty much the same way that someone without the disease can, having arthritis makes exercise a little more complicated.High-impact exercise, like running, jogging, and aerobics, can put too much stress on the joints, so doctors recommend against these activities. “They can hasten the arthritis process and cause injury,” says Westrich.
Instead, Vangsness recommends that his patients pursue one of three types of exercise that are particularly well suited for people with arthritis:
- Swimming
- Cycling (especially on a recumbent stationary bike, which is easier on knees and hips than a standard bike)
- Elliptical trainers
He adds that some of his extremely obese patients have gotten their weight loss started through gastric bypass or gastric banding surgery. “They start peeling off the pounds, and this tremendous loss of weight really knocks down their pain,” he says. “It’s like a whole new knee. And after losing that weight, they can exercise where they couldn’t before, strengthen their muscles, and further reduce pain.”
Thursday, November 11, 2010
Republic Pain Management knows how to throw a party!
Thank you to all who came to our GRAND opening party! we had so much fun with you all!
Hope you all went home with a flipbook to show your friends, had great food and plenty to drink while you checked out our stunning office.
Thank you for being our guest!
Tuesday, November 9, 2010
Republic Spine & Pain
A name does not define us. It does not change the deep desire to treat those in pain, our commitment to offering service that is inspired by the word ‘compassion’ and it does not change our devotion to educating patients on pain management.
Our Texas raised physicians are proud to serve you but we have changed our name.
We are now REPUBLIC SPINE & PAIN
Monday, November 8, 2010
Is your AUSTIN PAIN DOCTOR fellowship trained?
Picking your pain physician is an important part of the healing process.
Republic Spine and Pain is dedicated to increasing our understanding of pain, armed with skills focused on this, many more patients will benefit today than was possible when more senior doctors started their medical careers.
The specialty practice of pain management evolved greatly, largely through advances in post-operative pain control overseen by anesthesiologists. The job of an anesthesiologist expanded from providing anesthesia during surgery, pain control for women in labor, trauma patients, and other types of cases.
A fellowship is additional clinical training that a physician undertakes after completing a residency.
Dr Ostadian and Dr Yeh trained in interventional, interdisciplinary, acute, chronic, and cancer pain management on an inpatient and outpatient basis.The primary site for training is the Eugene McDermott Center for Pain Management (Pain Center), a prominent endowed center at UT Southwestern.
We know Patients have a choice when it comes to medical care and we appreciate patients choosing Republic Spine and Pain.
Besides the medical training our physicians have, it is their caring bedside manner that attracts patients.
It's the time our doctors spend with each patient and the fact that each patient visit is ALWAYS with a physician.
For more information, please visit our website or call our office to make an appointment
512 219 8787
Republic Spine and Pain is dedicated to increasing our understanding of pain, armed with skills focused on this, many more patients will benefit today than was possible when more senior doctors started their medical careers.
The specialty practice of pain management evolved greatly, largely through advances in post-operative pain control overseen by anesthesiologists. The job of an anesthesiologist expanded from providing anesthesia during surgery, pain control for women in labor, trauma patients, and other types of cases.
Fellowship training is the highest level of training available for doctors in any given subspecialty of medicine.
For example, a doctor finishes medical school, then goes to do an internship and a residency. A fellowship is an optional, additional level of training that takes his or her expertise one step higher.
Fellowship training exposes the doctor to the most complex medical cases and advanced treatments for medicine in their specialty area. Its important to make sure your physician is fellowship trained, but even more importantly where did they do their fellowship? All the physicians at Republic Spine and Pain did a fellowship an ACGME accredited university-based medical programs.
Dr Ostadian and Dr Yeh trained in interventional, interdisciplinary, acute, chronic, and cancer pain management on an inpatient and outpatient basis.The primary site for training is the Eugene McDermott Center for Pain Management (Pain Center), a prominent endowed center at UT Southwestern.
We know Patients have a choice when it comes to medical care and we appreciate patients choosing Republic Spine and Pain.
Besides the medical training our physicians have, it is their caring bedside manner that attracts patients.
It's the time our doctors spend with each patient and the fact that each patient visit is ALWAYS with a physician.
For more information, please visit our website or call our office to make an appointment
512 219 8787
Saturday, November 6, 2010
Finding the RIGHT Pain Management Physician
Picking your Pain Physician is an important part of the healing process.
Republic Spine & Pain is dedicated to continually increasing our understanding of pain. Armed with the skills gained from continued research focused on the mechanisms behind pain, the effects of pain on the whole person, and new treatment modalities which evidence has shown to be effective, many more patients will benefit today than was possible in the past when physicians were trained. Not too long ago, the medical field and the physicians who trained during that time had less understanding of all the reasons people experience pain, of the far-reaching consequences of pain on the body and the mind, and they were not aware of some of the new technologies and treatments that can be utilized today to alleviate pain, when learned through specialized training in Pain Management.
The specialty practice of Pain Management evolved greatly. This occurred largely through advances in post-operative pain control overseen by anesthesiologists. The job of an anesthesiologist expanded from providing anesthesia during surgery, typical pain control for women during labor, and to trauma patients.
Republic Spine & Pain is proud say all our physicians are Board Certified Anesthesiologists.
Fellowship training is the highest level of training available for a doctor in any given sub-specialty of medicine.
For example, a doctor first must complete medical school, then proceeds to an internship and residency program. After all of that extensive training in an area of the medical field , typically 7-9 years after an undergraduate degree is obtained, a fellowship is an additional specialised year that takes his or her expertise one step higher.
Fellowship training exposes a physician to the most complex medical cases and advanced treatments in medicine that are available in their specialty area. It is important to make sure that your physician is Fellowship-Trained; and even more importantly - where did they complete their fellowship? All of the physicians at Republic Spine & Pain completed a fellowship program at an ACGME accredited university-based medical program.
REMINDER: A fellowship is additional clinical training that a physician undertakes after completing a residency, to become highly specialized in their field. Wouldn't you want to go to a doctor who had the best knowledge and training to be able to effectively help you or your loved from all of the harmful effects of ongoing and/or severe pain? And improve their quality of life?
Dr Ostadian and Dr Yeh trained in interventional, interdisciplinary, acute, chronic, and cancer pain management in both inpatient and outpatient settings.The primary site for their training was the Eugene McDermott Center for Pain Management Pain Center, a prominent endowed center and ACGME accredited fellowship program at UT Southwestern.
Republic Spine & Pain is dedicated to continually increasing our understanding of pain. Armed with the skills gained from continued research focused on the mechanisms behind pain, the effects of pain on the whole person, and new treatment modalities which evidence has shown to be effective, many more patients will benefit today than was possible in the past when physicians were trained. Not too long ago, the medical field and the physicians who trained during that time had less understanding of all the reasons people experience pain, of the far-reaching consequences of pain on the body and the mind, and they were not aware of some of the new technologies and treatments that can be utilized today to alleviate pain, when learned through specialized training in Pain Management.
The specialty practice of Pain Management evolved greatly. This occurred largely through advances in post-operative pain control overseen by anesthesiologists. The job of an anesthesiologist expanded from providing anesthesia during surgery, typical pain control for women during labor, and to trauma patients.
Republic Spine & Pain is proud say all our physicians are Board Certified Anesthesiologists.
Fellowship training is the highest level of training available for a doctor in any given sub-specialty of medicine.
For example, a doctor first must complete medical school, then proceeds to an internship and residency program. After all of that extensive training in an area of the medical field , typically 7-9 years after an undergraduate degree is obtained, a fellowship is an additional specialised year that takes his or her expertise one step higher.
Fellowship training exposes a physician to the most complex medical cases and advanced treatments in medicine that are available in their specialty area. It is important to make sure that your physician is Fellowship-Trained; and even more importantly - where did they complete their fellowship? All of the physicians at Republic Spine & Pain completed a fellowship program at an ACGME accredited university-based medical program.
REMINDER: A fellowship is additional clinical training that a physician undertakes after completing a residency, to become highly specialized in their field. Wouldn't you want to go to a doctor who had the best knowledge and training to be able to effectively help you or your loved from all of the harmful effects of ongoing and/or severe pain? And improve their quality of life?
Dr Ostadian and Dr Yeh trained in interventional, interdisciplinary, acute, chronic, and cancer pain management in both inpatient and outpatient settings.The primary site for their training was the Eugene McDermott Center for Pain Management Pain Center, a prominent endowed center and ACGME accredited fellowship program at UT Southwestern.
Subscribe to:
Posts (Atom)


