- At some point in their lives, 80% of Americans will experience back pain.
- You can injure your back by coughing or sneezing.
- If you have a sprained or strained back—not a serious injury—use ice to help reduce swelling, muscle spasms, and pain for the first 24 to 48 hours after you injure your back.
- If you have a sprained or strained back-not a serious injury-use ice first. After 48 hours, switch to heat to warm and relax sore tissues.
- Good posture is one of the best ways to avoid straining your spine.
- Exercising on a regular basis helps you maintain a healthy spine.
- Each year, back pain costs Americans about $100 billion in medical bills, disability, and lost productivity.
To restore quality of life, to increase function, and to regain wholeness for patients suffering from chronic pain.
Friday, December 24, 2010
Why so I have Pain?
Wednesday, December 22, 2010
Merry Christmas From Republic Spine and Pain
Wishing all our patients a Wonderful Christmas.
We Hope the New Year brings you all wellness, joy and enlightenment.
Happy Holidays!
Sunday, December 19, 2010
Tips to Prevent Back Pain
In previous blogs we have dicussed the correct and incorrect way to lift objects and exercises to strengthen back muscles. Here are some TOP TIPS of things to be mindful of...
- Protecting Your Back in Bed
You'd think it would be difficult to injure your back while sleeping. While unconscious your muscles are relaxed and you're not lifting or carrying anything. But the truth is, if you have a bed that does not offer your back enough support, it could be the reason why you wake up with back-stiffness. Also, if you are in a position that is bad for your back and you stay in it for eight hours while you sleep, you could be damaging your back without knowing it.
- Protecting Your Back in the Morning
While you're getting ready in the morning to start your day there are a host of bad habits that could put stress on your back. For instance, when you stand at the sink, brushing your teeth, do you support your back? There's nothing like starting out your day on the right foot.
- Protecting Your Back in the Car
Many of us spend a significant portion of our days in the car. Strangely, little though is given to how comfortable we are in our cars, or what damage our car seats could be doing to our backs.
- Protecting Your Back at Work
Your office is like your home-away-from-home. Yet, almost not consideration is given to how comfortable you are while sitting at your desk. The wrong type of chair, a keyboard or monitor that is positioned at the wrong angle, or just sitting in one position for too long can all add up to significant back problems.
- Protecting Your Back While Exercising
It's a vicious cycle. If your back hurts, you will probably stop exercising. But if you stop exercising, you are more likely to injure your back. Even if your back is bothering you, it is important to get at least a little exercise. Movement keeps the joints in your back lubricated and loose.
- Stretches for Your Back
Keeping your back flexible is a big part of keeping your back injury-free. When your back tightens up, you are more likely to pull or strain a muscle.
- Exercises for Your Back
Though we told you earlier how to exercise without injuring your back, what we did not do is show you exercises to specifically strengthen your back. The muscles in your back not only support the spine, but they hold up your entire upper-body. Your back muscles need both strength and conditioning to perform their functions properly.
- Protecting Your Back While Lifting
Most people who throw out their back do so by attempting to lift an object incorrectly. Lifting puts more stress on your back than any other activity -- with the possible exception of carrying.
- Protecting Your Back When Moving Objects
Transporting or carrying an object may not provide the immediate, traumatic stress that comes when trying to lift an object, but it can do just as much damage to your back. There are several techniques you can employ to help you move objects that won't result in a trip to the emergency room.
- Diet and Back Pain
Watching what you can eat can also help protect your back. Most obviously, if you do not carry a lot of weight on your front, it will take a lot of strain off of your back muscles. But in addition to the benefits of maintaining a healthy weight, the right foods can also prevent back injuries. If you are tired and fatigued from lack of nutrition, you are much more likely to pull a muscle or acquire another back injury.
- Stress and Back Pain
Stress and tight muscles go together hand-in-hand. If you are carrying a lot tension in your upper back and shoulders, you are ripe for a back injury.
Thursday, December 16, 2010
Smoking and Back Pain
Low back pain affects 80 percent of us at some point in our lives. As a result, researchers are working diligently to determine what factors contribute to this pain. Some of the factors that have been identified include an occupation requiring a heavy physical workload, low levels of leisure physical activity, high body mass index, living in a small community, having a low educational level and being a smoker. While some of these factors may seem like common sense, some may be more surprising to you. The primary goal of this article is to present some evidence as to the effects smoking has on back pain and some possible explanations as to why.
It would seem logical that the more demand an activity or load places on the spine, the more likely it is that the spine may become injured. If the spine is injured, pain is likely to result. This is the obvious explanation as to why high body mass index and heavy occupational workloads tend to be associated with low back pain. However, an important factor with chronic loading of any part of the body is how well the body can recover or heal from the small damage caused by the loading. Ideally, the body heals a little stronger than it started and is more resistant to that same load in the future. If the body is not able to heal sufficiently, further injury develops. The key to healing is providing sufficient time between when the demand is placed on the body and the area of the body having enough blood supply to provide healing. An example of the time factor is a blister on your foot. Given enough time the blister will heal and the foot will be ready for taking stress once again. If the stress that created the blister is small and time is given between when the stress is applied, a callous forms instead of a blister. The body adapts instead of being injured. In the case of blood supply, think of the inside of your lip. This area has a rich blood supply and if cut will heal quite fast. The spine is similar. If it has a good blood supply, it will adapt to the physical demands placed on it. If the demand is too great, damage will occur.
One of the chief effects of smoking on the spine is that smoking contributes to atherosclerosis. Atherosclerosis is when plaque or other material builds up on the inside of blood vessels, causing decreased blood supply especially to areas that are fed by very small vessels. The bones and discs of the spine are supplied by these small vessels and are affected by atherosclerosis which decreases the spine’s ability to heal itself. This eventually leads to degeneration of the spine and the onset of pain. In this way, smoking increases the risk of developing atherosclerosis related to back pain [Source: Kaupplia, Leino-Arjas].
Also related to the spine’s ability to heal is the role of a bone cell called an osteoblast, a specialized cell the builds bone tissue. Nicotine is a major chemical in smoking that contributes to its addictive properties. However, nicotine also inhibits the activity of osteoblasts [Source: Glowacki]. Decreased osteoblast activity from nicotine causes the bones of the spine to have a reduced ability to rebuild. Over time, the bone is used up faster than it can be rebuilt causing osteoporosis and other degenerative conditions causing pain.
Another connection that has been made between smoking and low back pain is the message of pain itself. Smokers have been found to have higher ratings of pain than nonsmokers [Source: Ackerman, Scott, Vogt]. While the exact reasons for this are not entirely clear, it appears to have some connection with chemical interference with the body’s natural hormonal activity for pain detection. Essentially, the hormones and chemicals that help the body deal with pain are inhibited by smoking.
Other questions about smoking include whether smoking has an effect on intervertebral discs or on neck pain. At this time there is no conclusive evidence of smoking causing either of these conditions [Source: Gore, Leboeuf-Yde]. We may find that there is a link with further research. However, even if it is found that smoking does not cause disc problems or neck pain, the fact remains that smokers will tend to have more feelings of pain if there is an injury caused by something else.
The body is a remarkably resilient system. It can adapt and heal. However, it is also susceptible to harmful influences. It is up to each of us to take care of our own bodies and limit those harmful things by the choices we make. Smoking cessation, exercise and an improved diet are all personal decisions and habits that can be improved. Your body will thank you.
Sources
- Ackerman WE 3rd, Ahmad M. Effect of cigarette smoking on serum hydrocodone levels in chronic pain patients. J Ark Med Soc. 2007 Jul; 104(1): 19-21.
- Bjorck-van Dijken C, Fjellman-Wiklund A, Hildingsson C. Low back pain, lifestyle factors and physical activity: a population based-study. J Rehabil Med. 2008 Nov; 40(10):864-9.
- Freedman MK, Sauline MF, Overton EA, Holding MY, Kornbluth ID. Interventions in chronic pain management: approaches to medication and lifestyle in chronic pain syndromes. Arch Phys Med Rehabil. 2008 Mar; 89(3 Suppl 1):556-60.
- Glowacki J, Schulten AJ, Perrott D, Kaban LB. Nicotine impairs distraction osteogenesis in the rat mandible. Int J Oral Maxillofac Surg. 2008 Feb; 37(2):156-61.
- Gore DR, Carrera GF, Glaeser ST. Smoking and degenerative changes of the cervical spine: a roentgenographic study. Spine J. 2006 Sep-Oct; 6(5):557-60.
- Kaupplia LI. Atherosclerosis and disc degeneration/low back pain - a systematic review. Eur J Vasc Endovasc Surg. 2009 Mar 25.
- Leboeuf-Yde C, Kjaer P, Bendix T, Manniche C. Self-reported hard physical work combined with heavy smoking or overweight may result in so-called modic changes. BMC Musculoskelet Disord. 2008 Jan 14; 9:5.
- Leino-Arjas P, Solovieva S, Kirjonen J, Reunanen A, Riihimaki H. Cardiovascular risk factors and low-back pain in a long-term follow-up of industrial employees. Scand J Work Environ Health. 2006 Feb; 32(1): 12-19.
- Mikkonen P, Leino-Arjas P, Remes J, Zitting P, Taimela S, Karppinen J. Is smoking a risk factor for low back pain in adolescents? A prospective cohort study. Spine. 2008, Mar 1;33(5): 527-32.
- Scott SC, Goldberg MS, Mayo NE, Stock NE, Poltras B. The association between cigarette smoking and back pain in adults. Spine. 1999, Jun 1;24(11):1090-98.
- Vogt MT, Hanscom B, Lauerman WC, Kang JD. Influence of smoking on the health status of spinal patients: the National Spine Network database. Spine. 2002 Feb 1;27(3): 313-19.
For support groups in Austin to help quit smoking, visit these websites :
http://organizedwisdom.com/Smoking_Cessation_in_Austin
http://stopsmokingsimplified.com/SupportGroupsDetails.aspx
Monday, December 13, 2010
Be a Fan of Austin's Republic Spine and Pain on Facebook!
Facebookers! We value your support !
Follow Us on Twitter & Fan us on Facebook
Our patients are online researchers and we have got to keep up with you!
Our Austin Pain Clinic is becoming so Tech Savvy!
Friday, December 10, 2010
Pain Management Austin -
We are very blessed to work for 2 of Austins Best Pain Management Physicians.
They are always educating staff and patients on what is available to help patients not suffer and provide options for patients to choose from.
Wanted to share our Pain physicians Bio's from our website.
PHYSICIAN BIOGRAPHIES
Dr. Yeh and Dr. Ostadian met during their fellowship training in Dallas and realized they had a mutual vision for providing appropriate, compassionate and patient-centered care to those individuals suffering from chronic and acute pain. From there, they decided to create Republic Spine and Pain to treat those suffering from pain in the underserved areas of North Austin, Cedar Park, Round Rock and their surrounding communities.Dr. Yeh and Dr. Ostadian believe in a multi-disciplinary approach to pain management. This belief forms the cornerstone philosophy of Republic Spine and Pain’s strive to work with patients and their families to develop personalized care plans that utilize interventional techniques, medications, physical therapy, and minor surgery when indicated, to relieve pain and restore functionality.
Dr. Clement Yeh, MD
Dr. Clement Yeh has had the blessing of being a lifelong Texas resident. He was born in Dallas, TX and attended Arlington Martin High School. He then attended Baylor University on a Presidential and Premedical scholarship where he obtained a degree in biology and a minor in chemistry. In addition to being a member of Sigma Alpha Epsilon fraternity, he was also a 4-year starter on the Baylor men's soccer team and named the team's most valuable player his senior year.Dr. Yeh then later attended Texas Tech University School of Medicine for his medical education. During this time, he had the opportunity to complete his clinical clerkships in El Paso, TX where he had the immensely rewarding opportunity to mentor University of Texas at El Paso premedical students in guiding their career choices. This is also where his love of Mexican food was born.
Later, Dr. Yeh continued his medical education at Parkland Memorial Hospital and UT Southwestern Medical Center in Dallas, TX where he completed a residency in Anesthesiology. While a resident there, he published research in cardiovascular anesthesia as well as took the opportunity to present research posters at national anesthesiology meetings.
Although Dr. Yeh thoroughly enjoyed the fast-paced and intellectually stimulating environment that anesthesiology provided, his desire for a more traditional patient-physician relationship spurred him to pursue additional training in the field of pain medicine. He chose to remain at UT Southwestern Medical Center to complete his fellowship training in interventional pain management where he was trained in the latest interventional techniques and treatments for acute and chronic pain conditions and the importance of using a multidisciplinary-guided approach to treating pain. During this time, he was also able to present cutting edge research findings at national pain society meetings.Dr. Yeh is also a Board-Certified Anesthesiologist.
When not seeing patients in clinic or practicing anesthesiology part-time, Dr. Yeh can be found playing ultimate frisbee and soccer at Zilker park as well as wakeboarding and snowboarding when the seasons permit. Although he has spent the majority of his life in the Dallas area, he is now pleased to call our state’s wonderful capital home.
PROFESSIONAL MEMBERSHIPS
- Travis County Medical Society
- Texas Medical Association
- Texas Pain Society
Dr. Mahan Ostadian, DO
Dr. Mahan Ostadian considers himself a Texas native since his early college years. He attended the University of Texas in Austin where he completed his premedical training and obtained a degree in biology. During this time, he remained active in the community while volunteering in the emergency room at Round Rock Community Hospital. He also continued his goal of becoming a physician by staying involved in Alpha Epsilon Delta pre-medical honor society at the university.Dr. Ostadian left Austin to attend University of North Texas Health Sciences Center - Texas College of Osteopathic Medicine in Fort Worth to complete his medical degree. While obtaining a solid foundation in the basic sciences, he also learned the interrelationship of the body's nerves, muscles, bones, and organs as well as the importance of treating the whole person. He was selected to the Dean’s List for academic excellence during this time.
Next, Dr. Ostadian continued his medical training through completing a residency in Anesthesiology at Scott and White Memorial Hospital. He remained on staff as an Assistant Professor of Anesthesiology there after his residency and was heavily involved as part of the hospital’s pain management team in helping treat patients’ post-operative pain. Currently, he enjoys his continued involvement at Scott and White in resident education.
While working as faculty at Scott and White Memorial Hospital, Dr. Ostadian decided to pursue fellowship training in interventional pain management from the respected UT Southwestern School of Medicine and Parkland Memorial Hospital in Dallas. During his fellowship training, he was involved in several research projects and presented research posters at national pain management conferences. Dr. Ostadian is a Board-Certified Anesthesiologist with advanced training in the latest interventional techniques and treatments for acute and chronic pain conditions.
Dr. Ostadian was thrilled about returning to Austin with his wife Mona, and their daughter Alana, and hopes to make a difference in the community. Dr. Ostadian is a huge college football fan and hopes his daughter will someday have the same passion that he has for Longhorn football. He is also excited to join with Dr. Yeh who shares his goals of providing exceptional compassionate care to all of their patients.
PROFESSIONAL MEMBERSHIPS
- American Society of Anesthesiologists
- American Medical Association
- Travis County Medical Society
- American Society of Regional Anesthesia and Pain Management
- Texas Medical Association
Wednesday, December 8, 2010
Tuesday, December 7, 2010
Austin Pain Clinic - What Makes Us Different?
We're devoted exclusively to Austin Pain Management Patients.
Republic Spine and Pain is devoted exclusively to advanced interventional pain management.
Our physicians offer patients a variety of interventional procedure options in an effort to avoid or reduce medication needs. Minimally invasive procedures are beneficial in two ways: First, interventions can be helpful in precisely identifying the source of the pain. Second, interventions can frequently provide long-term pain relief without surgery.
We utilize advanced imaging technology to ensure that pain relief is delivered precisely where patients need it most. If through the diagnosis process we determine that a patient needs a different treatment, we have a vast referral network to other preeminent specialists in Cedar Park, Round Rock & Austin. Our doctors may also refer you to other, non-physician specialists for additional care, such as physical therapy, occupational therapy or home health care. We will share information frequently with each of the other member team, to ensure that are all working together to provide you with the best possible relief of your pain.
Our Pain Management physicians and staff have many years of experience in caring for people struggling with chronic pain. If you haven’t found success in managing your chronic pain, please consider calling Republic Pain ( 512 219 8787 ).
Referrals to Pain Management are not generally required for office visits unless specified by your insurance company.
Republic Spine and Pain is devoted exclusively to advanced interventional pain management.
Our physicians offer patients a variety of interventional procedure options in an effort to avoid or reduce medication needs. Minimally invasive procedures are beneficial in two ways: First, interventions can be helpful in precisely identifying the source of the pain. Second, interventions can frequently provide long-term pain relief without surgery.
We utilize advanced imaging technology to ensure that pain relief is delivered precisely where patients need it most. If through the diagnosis process we determine that a patient needs a different treatment, we have a vast referral network to other preeminent specialists in Cedar Park, Round Rock & Austin. Our doctors may also refer you to other, non-physician specialists for additional care, such as physical therapy, occupational therapy or home health care. We will share information frequently with each of the other member team, to ensure that are all working together to provide you with the best possible relief of your pain.
Our Pain Management physicians and staff have many years of experience in caring for people struggling with chronic pain. If you haven’t found success in managing your chronic pain, please consider calling Republic Pain ( 512 219 8787 ).
Referrals to Pain Management are not generally required for office visits unless specified by your insurance company.
You don’t want to live in pain, and you don’t have to.
Please call us today.
Sunday, December 5, 2010
Vertebroplasty Procedure Animation
Vertebroplasty is a procedure that offers relief to patients suffering prolonged and debilitating pain from compression fractures in the spinal vertebrae. It involves injecting bone cement into the vertebrae to stabilize fractures, and results in significant pain relief and restoration of mobility in many patients.
To learn more click on the video link or ask our physicians on your consultation appointment.
To learn more click on the video link or ask our physicians on your consultation appointment.
Friday, December 3, 2010
Naomi Judd Offers Support to Those Living With Chronic Pain
She is now a spokesperson for the national education program Partners Against Pain.
Sunday November 21st, 2010
(NewsUSA) - It may surprise you to learn that before she became a country music icon, Naomi Judd was a critical care nurse. Unlike facing a stadium full of adoring fans, as a nurse she witnessed the daily challenges faced by people with chronic pain and those who care for them.
More recently, Judd watched a dear friend suffer from excruciating pain during his battle with pancreatic cancer. Because he was an educated and empowered patient, he received excellent pain management and was able to live his remaining days to the fullest.
As a spokesperson for the national education program Partners Against Pain, Judd now has 50 million reasons to let others know that they don't need to suffer in silence. That's because the latest statistics show that more than 50 million Americans live with pain, making it one of the top reasons people seek medical care.
Judd is encouraging people with pain and their caregivers to learn as much as they can about proper pain management. "From day to day, pain can limit your ability to enjoy your work, your hobbies -- even rob you of the simple joys of hugging someone you love," says Judd.
Each person's pain is unique and different. In many cases, managing pain requires an integrative approach that combines prescription medicine with complementary techniques such as physical therapy, acupuncture and massage.
Judd wants people to know the journey to appropriate pain management can begin with a visit to the recently updated Partners Against Pain website (http://www.partnersagainstpain.com/). The new, user-friendly layout features customized sections for patients, caregivers and healthcare professionals that make it easy find information about various painful conditions, including arthritis, cancer pain and low back pain. Special downloadable features -- such as a Patient Comfort Assessment Guide with a daily pain diary and pain management log -- are also available, along with links to other pain education and advocacy groups.
The website also contains valuable information and tools to help family caregivers meet the unique challenges of caring for loved ones coping with chronic pain.
Partners Against Pain is a national education program provided by Purdue Pharma
Monday, November 29, 2010
FDA approves Botox as migraine preventive
Helpful news for patients suffering from daily migraines 15 days or more in a month that last 4 hours or more! Botox -- Orginally known for smoothing out wrinkles on the face -- has been approved by the FDA to treat chronic migraines in adults. Call us to see how we can help migraine sufferers and work with your insurance to see if the procedure is covered. 512 219 8787
(CNN) -- Federal health authorities on Friday approved Botox injections for the prevention of chronic migraines in adults, an advance experts described as "modest."
In a statement, the Food and Drug Administration recommended Botox be injected approximately every three months around the head and neck to dull future headache symptoms.
The drug -- whose generic name is onabotulinumtoxinA -- has not been shown to work against migraines that occur 14 days or fewer per month, nor has it been shown to work for other forms of headache, said the statement.
Experiencing a migraine on most days "is one of the most disabling forms of headache," said Dr. Russell Katz, of the Division of Neurology Products in the FDA's Center for Drug Evaluation and Research. "This condition can greatly affect family, work, and social life, so it is important to have a variety of effective treatment options available."
Migraines, an intense pulsing or throbbing pain in one area of the head, are often accompanied by nausea, vomiting and sensitivity to light and sound, doctors say. Chronic migraines are defined as those that occur on 15 days or more for more than four hours per day.
The drug, made by Allergan, Inc., of Irvine, California, was approved last month in Britain for the same purpose.
The two company-funded studies submitted to the FDA involved 1,384 adults from 122 study sites in Europe and North America. They found that after six months, patients who got the drug experienced 7.8 and 9.2 fewer days of migraine than they had before the studies started. Those who got injections of placebo (sugar pill) experienced 6.4 and 6.9 fewer headache days.
Over those six months, patients on the drug experienced 107 and 134 fewer hours of headache, versus a reduction of 70 and 95 hours for those on placebo, according to the studies.
"The benefits are modest when you look at the overall results," said Dr. Elizabeth W. Loder, associate professor of neurology at Harvard Medical School and the chief of the division of headaches in the Department of Neurology at the Brigham and Women's Hospital in Boston. Loder was involved in an Allergan-funded trial several years ago but has no current relationship with the company.
"But, of course, within those results, there are always patients who do much better than the average and there are patients who don't have any benefit," she said.
Still, she added, "It will provide more options for patients who currently have very few forms of treatment available to them ... when you are dealing with a problem like this, even modest improvement can mean the difference between being able to go to work and not being able to function very well."
Dr. Joel Saper, director of the Michigan Head Pain and Neurological Institute and clinical professor of neurology at Michigan State University, said he has been using the drug for that purpose for more than a decade, even though it was not approved for it.
The FDA's approval will likely mean that insurance companies will pick up the tab for it now, he said. Saper, who has also participated in Allergan-funded trials, predicted "certain subsets of people will get dramatic results."
The most common adverse reactions reported by chronic migraine patients being treated with Botox were neck pain and headache, the FDA said.
About 1 percent of patients on the drug (versus 0.3 percent of those on placebo) found that their migraines worsened so much they had to be hospitalized, but it was generally well-tolerated, the company said.
In each study, less than 2 percent of patients dropped out of the study due to an adverse event.
The drug labeling warns that the effects of the botulinum toxin may spread beyond where it is injected, causing symptoms that may include life-threatening difficulties swallowing and breathing.
Botox is sold to doctors in 200-unit vials that cost $1,050, said Cyrstal Muilenburg, spokeswoman for Allergan. Last year, the drug had sales of $1.3 billion, she said.
Doctors gave administered a total of 155 units to each migraine patient in 31 injections into muscles of the head and neck, she said. The treatment was repeated at three-month intervals.
Some 3.2 million Americans are estimated to suffer from chronic migraine, though some 80 percent of them have never been diagnosed as having the disease, the company said.
The World Health Organization ranks migraine as the 19th most disabling disease. Women are three times as likely as men to suffer from migraines, which are also linked to depression and anxiety.
The drug is the same chemical entity that was approved 21 years ago for the treatment of strabismus and blepharospasm, two eye-muscle disorders.
Since then, regulators in some 80 countries have approved it for 21 different indications, including treatment of the abnormal head position and neck pain associated with cervical dystonia in adults, symptoms of severe underarm sweatingand treatment of increased muscle stiffness in elbow, wrist and finger muscles in adults with upper-limb spasticity.
By Tom Watkins, CNN
(CNN) -- Federal health authorities on Friday approved Botox injections for the prevention of chronic migraines in adults, an advance experts described as "modest."
In a statement, the Food and Drug Administration recommended Botox be injected approximately every three months around the head and neck to dull future headache symptoms.
The drug -- whose generic name is onabotulinumtoxinA -- has not been shown to work against migraines that occur 14 days or fewer per month, nor has it been shown to work for other forms of headache, said the statement.
Experiencing a migraine on most days "is one of the most disabling forms of headache," said Dr. Russell Katz, of the Division of Neurology Products in the FDA's Center for Drug Evaluation and Research. "This condition can greatly affect family, work, and social life, so it is important to have a variety of effective treatment options available."
Migraines, an intense pulsing or throbbing pain in one area of the head, are often accompanied by nausea, vomiting and sensitivity to light and sound, doctors say. Chronic migraines are defined as those that occur on 15 days or more for more than four hours per day.
The drug, made by Allergan, Inc., of Irvine, California, was approved last month in Britain for the same purpose.
The two company-funded studies submitted to the FDA involved 1,384 adults from 122 study sites in Europe and North America. They found that after six months, patients who got the drug experienced 7.8 and 9.2 fewer days of migraine than they had before the studies started. Those who got injections of placebo (sugar pill) experienced 6.4 and 6.9 fewer headache days.
Over those six months, patients on the drug experienced 107 and 134 fewer hours of headache, versus a reduction of 70 and 95 hours for those on placebo, according to the studies.
"The benefits are modest when you look at the overall results," said Dr. Elizabeth W. Loder, associate professor of neurology at Harvard Medical School and the chief of the division of headaches in the Department of Neurology at the Brigham and Women's Hospital in Boston. Loder was involved in an Allergan-funded trial several years ago but has no current relationship with the company.
"But, of course, within those results, there are always patients who do much better than the average and there are patients who don't have any benefit," she said.
Still, she added, "It will provide more options for patients who currently have very few forms of treatment available to them ... when you are dealing with a problem like this, even modest improvement can mean the difference between being able to go to work and not being able to function very well."
Dr. Joel Saper, director of the Michigan Head Pain and Neurological Institute and clinical professor of neurology at Michigan State University, said he has been using the drug for that purpose for more than a decade, even though it was not approved for it.
The FDA's approval will likely mean that insurance companies will pick up the tab for it now, he said. Saper, who has also participated in Allergan-funded trials, predicted "certain subsets of people will get dramatic results."
The most common adverse reactions reported by chronic migraine patients being treated with Botox were neck pain and headache, the FDA said.
About 1 percent of patients on the drug (versus 0.3 percent of those on placebo) found that their migraines worsened so much they had to be hospitalized, but it was generally well-tolerated, the company said.
In each study, less than 2 percent of patients dropped out of the study due to an adverse event.
The drug labeling warns that the effects of the botulinum toxin may spread beyond where it is injected, causing symptoms that may include life-threatening difficulties swallowing and breathing.
Botox is sold to doctors in 200-unit vials that cost $1,050, said Cyrstal Muilenburg, spokeswoman for Allergan. Last year, the drug had sales of $1.3 billion, she said.
Doctors gave administered a total of 155 units to each migraine patient in 31 injections into muscles of the head and neck, she said. The treatment was repeated at three-month intervals.
Some 3.2 million Americans are estimated to suffer from chronic migraine, though some 80 percent of them have never been diagnosed as having the disease, the company said.
The World Health Organization ranks migraine as the 19th most disabling disease. Women are three times as likely as men to suffer from migraines, which are also linked to depression and anxiety.
The drug is the same chemical entity that was approved 21 years ago for the treatment of strabismus and blepharospasm, two eye-muscle disorders.
Since then, regulators in some 80 countries have approved it for 21 different indications, including treatment of the abnormal head position and neck pain associated with cervical dystonia in adults, symptoms of severe underarm sweatingand treatment of increased muscle stiffness in elbow, wrist and finger muscles in adults with upper-limb spasticity.
Wednesday, November 24, 2010
Happy Thanksgiving
We have so much to be thankful for this season.
Republic Spine and Pain would like to wish Austin, Cedar Park, Leander, Lago Vista and Round Rock a wonderful holiday with your loved ones.
Best wishes in health and happiness,
Dr Yeh, Dr Ostadian, Jamika, Maria & Mona
Republic Spine and Pain would like to wish Austin, Cedar Park, Leander, Lago Vista and Round Rock a wonderful holiday with your loved ones.
Best wishes in health and happiness,
Dr Yeh, Dr Ostadian, Jamika, Maria & Mona
Monday, November 22, 2010
FDA pulls common pain med off the market
Important Pain Managament News - If you are a patient at Republic Spine and Pain and have questions about the Pain Medications you are currently taking please call our staff at Republic Pain. Making sure Austin Pain Management patients are well informed about their medications is important to us.
By the CNN Wire Staff
By the CNN Wire Staff
November 19, 2010 2:40 p.m. EST
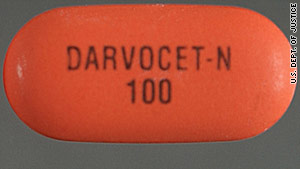
Washington (CNN) -- The pharmaceutical company that makes the prescription pain medications Darvon and Darvocet has agreed to withdraw the drugs from the U.S. market at the request of the U.S. Food and Drug Administration, the FDA said Friday.
"We recommend to physicians stop prescribing the drugs. As for patients, do not stop taking it, but we urge you to contact your health care professional. Do not delay," said Gerald Dal Pan, director of the FDA's Office of Surveillance and Epidemiology.
Xanodyne Pharmaceuticals Inc. manufactures Darvon and Darvocet, two brand name versions of propoxyphene. The FDA also asked generic makers of the pain medicine to voluntarily remove their products.
The decision to remove the drug came after the FDA reviewed a new trial study that looked at the drug's impact on heart rhythms.
"The drug's effectiveness in reducing pain is no longer enough to outweigh the drug's serious potential heart risks," the FDA said in a statement released Friday.
Propoxyphene, first approved by the FDA in 1957, is an opioid used to treat mild to moderate pain. It is sold under various names both alone, such as Darvon, or in combination with acetaminophen, such as Darvocet.Since 1978, the FDA has received two requests to remove propoxyphene from the market, but concluded that the benefits of propoxyphene for pain relief at recommended doses outweighed the safety risks.
Saturday, November 20, 2010
Could Losing Weight Help Arthritis Pain?
Our Pain Management physicians strongly believe that any treatment plan should be combined with exercise when possible. There are a great selection of parks, gyms, physical therapists in Austin to support your decision to get active.
WebMD Feature
WebMD Feature
By Gina Shaw
Reviewed By Brunilda Nazario, MD
For 12 years, Robin Lutchansky spent most of her time in a wheelchair. The pain from her severe osteoarthritis, first diagnosed in her early 30s, made it difficult to walk more than short distances.
Today, Lutchansky is out of the wheelchair and back at work as a public relations representative for a high-tech firm, and says that her daily pain levels have gone from an 8 or a 9 to a 1. “It’s amazing. It’s a new life. I had no idea it was possible.”
“When we walk, when we go up and down stairs, or get into or out of a chair or car, we can put three to five times our body weight, and sometimes more, on the joints,” says Geoffrey Westrich, attending orthopedic surgeon and Director of Joint Replacement Research at the Hospital for Special Surgery in New York. “So if you’re 50 pounds overweight, you’re putting around 250 pounds of increased stress across your knees and hips.”
Over time, that extra weight makes you much more prone to developing arthritis and can cause arthritis to progress much more rapidly, leading to much more pain once it has developed.
Fortunately, the same principle works in reverse. “For every pound people lose, they lose 3 pounds of stress across their knee and 6 pounds of stress on their hip, on average,” says Westrich.
Jane Angelich, a 58-year-old California businesswoman, has lost 33 pounds on Weight Watchers.
“What a difference!” she says. “It starts when I get out of bed in the morning. No more limping around and groaning for the first few minutes. Instead of finding excuses to sit on my couch instead of walking around, I now walk the equivalent of a 5k without any issues and can even function the next day!”
High-impact exercise, like running, jogging, and aerobics, can put too much stress on the joints, so doctors recommend against these activities. “They can hasten the arthritis process and cause injury,” says Westrich.
Instead, Vangsness recommends that his patients pursue one of three types of exercise that are particularly well suited for people with arthritis:
He adds that some of his extremely obese patients have gotten their weight loss started through gastric bypass or gastric banding surgery. “They start peeling off the pounds, and this tremendous loss of weight really knocks down their pain,” he says. “It’s like a whole new knee. And after losing that weight, they can exercise where they couldn’t before, strengthen their muscles, and further reduce pain.”
Then, a little over three years ago, Lutchansky found her way to a pain management clinic that taught her how to exercise -- first, teaching her how to walk again. Over the next three years, Lutchansky, now 51, gradually lost nearly 100 pounds with calorie reduction and exercise.
“I did it slowly. I started out just lifting 2-pound weights, and I walked in the pool every day,” she says.Today, Lutchansky is out of the wheelchair and back at work as a public relations representative for a high-tech firm, and says that her daily pain levels have gone from an 8 or a 9 to a 1. “It’s amazing. It’s a new life. I had no idea it was possible.”
What Weight Does to Your Joints
If you are at all overweight, one of the best ways to reduce osteoarthritis pain is by taking off excess pounds. Being overweight increases the load that you put on your joints -- your knees, your hips, your ankle -- with every step you take.“When we walk, when we go up and down stairs, or get into or out of a chair or car, we can put three to five times our body weight, and sometimes more, on the joints,” says Geoffrey Westrich, attending orthopedic surgeon and Director of Joint Replacement Research at the Hospital for Special Surgery in New York. “So if you’re 50 pounds overweight, you’re putting around 250 pounds of increased stress across your knees and hips.”
Over time, that extra weight makes you much more prone to developing arthritis and can cause arthritis to progress much more rapidly, leading to much more pain once it has developed.
Fortunately, the same principle works in reverse. “For every pound people lose, they lose 3 pounds of stress across their knee and 6 pounds of stress on their hip, on average,” says Westrich.
Small Steps, Big Changes
You don’t have to lose 100 pounds, like Lutchansky, to see a difference in your pain levels. C. Thomas Vangsness, Jr., MD, professor of orthopaedic surgery and chief of sports medicine at the Keck School of Medicine at the University of Southern California, says most of his arthritis patients who lose weight notice that their pain is diminishing after losing about 20 pounds.Jane Angelich, a 58-year-old California businesswoman, has lost 33 pounds on Weight Watchers.
“What a difference!” she says. “It starts when I get out of bed in the morning. No more limping around and groaning for the first few minutes. Instead of finding excuses to sit on my couch instead of walking around, I now walk the equivalent of a 5k without any issues and can even function the next day!”
Small Steps, Big Changes continued...
Losing weight cannot repair the damage that’s already been done to your joints by arthritis, but in addition to decreasing your pain, it can also help to slow down the further progression of the disease. One study found that knee osteoarthritis in obese men would decrease by 21.5% if they lost enough weight to be categorized as merely overweight; for women, arthritis would decrease by 31%.
“The damage is already done, and arthritis is a progressive process,” says Westrich. “But weight loss can be tremendously helpful in alleviating pain, allowing greater function, and prolonging the period of time before someone needs joint replacement surgery.”
And if you haven’t developed arthritis but you’re worried about it, losing excess weight can significantly lower your risk. If you’re significantly overweight, every 11 pounds you lose cuts your risk of developing arthritis by more than 50%.Making It Happen
The best way to lose weight, any doctor will tell you, is to eat less, eat healthy foods, and exercise more. But while someone with arthritis can start to change their eating habits in pretty much the same way that someone without the disease can, having arthritis makes exercise a little more complicated.High-impact exercise, like running, jogging, and aerobics, can put too much stress on the joints, so doctors recommend against these activities. “They can hasten the arthritis process and cause injury,” says Westrich.
Instead, Vangsness recommends that his patients pursue one of three types of exercise that are particularly well suited for people with arthritis:
- Swimming
- Cycling (especially on a recumbent stationary bike, which is easier on knees and hips than a standard bike)
- Elliptical trainers
He adds that some of his extremely obese patients have gotten their weight loss started through gastric bypass or gastric banding surgery. “They start peeling off the pounds, and this tremendous loss of weight really knocks down their pain,” he says. “It’s like a whole new knee. And after losing that weight, they can exercise where they couldn’t before, strengthen their muscles, and further reduce pain.”
Thursday, November 11, 2010
Republic Pain Management knows how to throw a party!
Thank you to all who came to our GRAND opening party! we had so much fun with you all!
Hope you all went home with a flipbook to show your friends, had great food and plenty to drink while you checked out our stunning office.
Thank you for being our guest!
Tuesday, November 9, 2010
Republic Spine & Pain
A name does not define us. It does not change the deep desire to treat those in pain, our commitment to offering service that is inspired by the word ‘compassion’ and it does not change our devotion to educating patients on pain management.
Our Texas raised physicians are proud to serve you but we have changed our name.
We are now REPUBLIC SPINE & PAIN
Monday, November 8, 2010
Is your AUSTIN PAIN DOCTOR fellowship trained?
Picking your pain physician is an important part of the healing process.
Republic Spine and Pain is dedicated to increasing our understanding of pain, armed with skills focused on this, many more patients will benefit today than was possible when more senior doctors started their medical careers.
The specialty practice of pain management evolved greatly, largely through advances in post-operative pain control overseen by anesthesiologists. The job of an anesthesiologist expanded from providing anesthesia during surgery, pain control for women in labor, trauma patients, and other types of cases.
A fellowship is additional clinical training that a physician undertakes after completing a residency.
Dr Ostadian and Dr Yeh trained in interventional, interdisciplinary, acute, chronic, and cancer pain management on an inpatient and outpatient basis.The primary site for training is the Eugene McDermott Center for Pain Management (Pain Center), a prominent endowed center at UT Southwestern.
We know Patients have a choice when it comes to medical care and we appreciate patients choosing Republic Spine and Pain.
Besides the medical training our physicians have, it is their caring bedside manner that attracts patients.
It's the time our doctors spend with each patient and the fact that each patient visit is ALWAYS with a physician.
For more information, please visit our website or call our office to make an appointment
512 219 8787
Republic Spine and Pain is dedicated to increasing our understanding of pain, armed with skills focused on this, many more patients will benefit today than was possible when more senior doctors started their medical careers.
The specialty practice of pain management evolved greatly, largely through advances in post-operative pain control overseen by anesthesiologists. The job of an anesthesiologist expanded from providing anesthesia during surgery, pain control for women in labor, trauma patients, and other types of cases.
Fellowship training is the highest level of training available for doctors in any given subspecialty of medicine.
For example, a doctor finishes medical school, then goes to do an internship and a residency. A fellowship is an optional, additional level of training that takes his or her expertise one step higher.
Fellowship training exposes the doctor to the most complex medical cases and advanced treatments for medicine in their specialty area. Its important to make sure your physician is fellowship trained, but even more importantly where did they do their fellowship? All the physicians at Republic Spine and Pain did a fellowship an ACGME accredited university-based medical programs.
Dr Ostadian and Dr Yeh trained in interventional, interdisciplinary, acute, chronic, and cancer pain management on an inpatient and outpatient basis.The primary site for training is the Eugene McDermott Center for Pain Management (Pain Center), a prominent endowed center at UT Southwestern.
We know Patients have a choice when it comes to medical care and we appreciate patients choosing Republic Spine and Pain.
Besides the medical training our physicians have, it is their caring bedside manner that attracts patients.
It's the time our doctors spend with each patient and the fact that each patient visit is ALWAYS with a physician.
For more information, please visit our website or call our office to make an appointment
512 219 8787
Saturday, November 6, 2010
Finding the RIGHT Pain Management Physician
Picking your Pain Physician is an important part of the healing process.
Republic Spine & Pain is dedicated to continually increasing our understanding of pain. Armed with the skills gained from continued research focused on the mechanisms behind pain, the effects of pain on the whole person, and new treatment modalities which evidence has shown to be effective, many more patients will benefit today than was possible in the past when physicians were trained. Not too long ago, the medical field and the physicians who trained during that time had less understanding of all the reasons people experience pain, of the far-reaching consequences of pain on the body and the mind, and they were not aware of some of the new technologies and treatments that can be utilized today to alleviate pain, when learned through specialized training in Pain Management.
The specialty practice of Pain Management evolved greatly. This occurred largely through advances in post-operative pain control overseen by anesthesiologists. The job of an anesthesiologist expanded from providing anesthesia during surgery, typical pain control for women during labor, and to trauma patients.
Republic Spine & Pain is proud say all our physicians are Board Certified Anesthesiologists.
Fellowship training is the highest level of training available for a doctor in any given sub-specialty of medicine.
For example, a doctor first must complete medical school, then proceeds to an internship and residency program. After all of that extensive training in an area of the medical field , typically 7-9 years after an undergraduate degree is obtained, a fellowship is an additional specialised year that takes his or her expertise one step higher.
Fellowship training exposes a physician to the most complex medical cases and advanced treatments in medicine that are available in their specialty area. It is important to make sure that your physician is Fellowship-Trained; and even more importantly - where did they complete their fellowship? All of the physicians at Republic Spine & Pain completed a fellowship program at an ACGME accredited university-based medical program.
REMINDER: A fellowship is additional clinical training that a physician undertakes after completing a residency, to become highly specialized in their field. Wouldn't you want to go to a doctor who had the best knowledge and training to be able to effectively help you or your loved from all of the harmful effects of ongoing and/or severe pain? And improve their quality of life?
Dr Ostadian and Dr Yeh trained in interventional, interdisciplinary, acute, chronic, and cancer pain management in both inpatient and outpatient settings.The primary site for their training was the Eugene McDermott Center for Pain Management Pain Center, a prominent endowed center and ACGME accredited fellowship program at UT Southwestern.
Republic Spine & Pain is dedicated to continually increasing our understanding of pain. Armed with the skills gained from continued research focused on the mechanisms behind pain, the effects of pain on the whole person, and new treatment modalities which evidence has shown to be effective, many more patients will benefit today than was possible in the past when physicians were trained. Not too long ago, the medical field and the physicians who trained during that time had less understanding of all the reasons people experience pain, of the far-reaching consequences of pain on the body and the mind, and they were not aware of some of the new technologies and treatments that can be utilized today to alleviate pain, when learned through specialized training in Pain Management.
The specialty practice of Pain Management evolved greatly. This occurred largely through advances in post-operative pain control overseen by anesthesiologists. The job of an anesthesiologist expanded from providing anesthesia during surgery, typical pain control for women during labor, and to trauma patients.
Republic Spine & Pain is proud say all our physicians are Board Certified Anesthesiologists.
Fellowship training is the highest level of training available for a doctor in any given sub-specialty of medicine.
For example, a doctor first must complete medical school, then proceeds to an internship and residency program. After all of that extensive training in an area of the medical field , typically 7-9 years after an undergraduate degree is obtained, a fellowship is an additional specialised year that takes his or her expertise one step higher.
Fellowship training exposes a physician to the most complex medical cases and advanced treatments in medicine that are available in their specialty area. It is important to make sure that your physician is Fellowship-Trained; and even more importantly - where did they complete their fellowship? All of the physicians at Republic Spine & Pain completed a fellowship program at an ACGME accredited university-based medical program.
REMINDER: A fellowship is additional clinical training that a physician undertakes after completing a residency, to become highly specialized in their field. Wouldn't you want to go to a doctor who had the best knowledge and training to be able to effectively help you or your loved from all of the harmful effects of ongoing and/or severe pain? And improve their quality of life?
Dr Ostadian and Dr Yeh trained in interventional, interdisciplinary, acute, chronic, and cancer pain management in both inpatient and outpatient settings.The primary site for their training was the Eugene McDermott Center for Pain Management Pain Center, a prominent endowed center and ACGME accredited fellowship program at UT Southwestern.
Friday, October 22, 2010
Spinal Cord Stimulation
By Medtronics
Spinal cord stimulation alleviates pain by electrically activating pain-inhibiting neuronal circuits in the dorsal horn and inducing a tingling sensation (paresthesia) that masks the sensations of pain.
Indications
A Medtronic implantable neurostimulation system is indicated for spinal cord stimulation (SCS) as an aid in the management of chronic, intractable pain of the trunk and/or limbs—including unilateral or bilateral pain associated with the following conditions:
- Failed Back Syndrome (FBS) or low back syndrome or failed back
- Radicular pain syndrome or radiculopathies resulting in pain secondary to FBSS or herniated disk
- Postlaminectomy pain
- Multiple back operations
- Unsuccessful disk surgery
- Degenerative Disk Disease (DDD)/herniated disk pain refractory to conservative and surgical therapies
- Peripheral causalgia
- Epidural fibrosis
- Arachnoiditis or lumbar adhesive arachnoiditis
- Complex Regional Pain Syndrome (CRPS), Reflex Sympathetic Dystrophy (RSD), or causalgia
How Spinal Cord Stimulation Treats Chronic Pain
Spinal cord stimulation involves the delivery of mild electrical signals to the epidural space. Pain signals are "masked" by the perception of a tingling sensation (parasthesia) in the area where the pain was felt.Published studies have shown that when used by carefully selected chronic pain patients, neurostimulation may:
- Effectively improve pain relief (a majority of patients may experience at least a 50% reduction in pain)2-4
- Increase activity levels2-5
- Reduce the use of narcotic medications3-5
- Lead to reduced hospitalizations and surgical procedures, reduced health care costs, greater independence, and improved quality of life2-4
Additionally, spinal cord stimulation offers the following advantages:
- Screening trial allows testing of a patient's response before a full implant
- Patient control within physician-set limits
- Non-destructive procedure compared with surgical alternatives
Monday, October 18, 2010
Technique for Lifting Heavy Objects
Many back problems occur not because the object is too heavy but rather because of the way it was lifted.
Most people go through life leaning forward to lift ... and the spine takes the full brunt of the force!
It doesnt matter how young or old you may be. Its important everyone uses safe techniques to prevent strain to your back.
Here are a few things to remember next time you offer to move something.
Most people go through life leaning forward to lift ... and the spine takes the full brunt of the force!
It doesnt matter how young or old you may be. Its important everyone uses safe techniques to prevent strain to your back.
Here are a few things to remember next time you offer to move something.
- The first step to lifting a heavy object safely is to get as close to it as you can. Ideally, the object should be underneath you.
- Next, take a wide stance. Legs should be wider than shoulders, with your weight anchored firmly into the ground or floor.
- Try different foot positions until you find the one that feels the most stable and comfortable. Try putting your left foot front, then your right. Or keep them parallel, but widen your stance. Once you have found your comfort level, get ready to use that position.
- Bend your knees and lift the object from underneath. You will be using the muscles in your hips and legs to do the heavy work. Avoid bending at the waist, which can cause you to injure a disk or strain your back.
- If you are lifting an unwieldy object, like a heavy bag of soil, get someone to help you. Taking a chance on lifting it is not worth the risk to your back.
- A trick for making sure you're lifting objects safely: Keep a long spine. Think about a line that goes from your head through your spine all the way down to your coccyx bone. Your body should stay in that position when lifting.
- One way to prepare your spine and find "the line" easily is to do the cat-cow yoga stretch. It will take you through arching and rounding your spine, warming it up and helping you to become more aware of the position of your back.
- Keeping your arms close to your body can help ensure that you're lifting an object safely. This will help keep the lifting efficient, helping you avoid shoulder, arm and back strain.
- When lifting your object, keep your knees in line with your toes. This will help you avoid knee strain, now that you are using hips and knees instead of your back. Don't let your knees drop inward or outward -- this will help your body stay aligned during the movement.
Monday, October 11, 2010
What exercise can I do to reduce low back pain?
Dr Ostadian and Dr Yeh believe it important to exercise daily and make sure physical activity is part of a your regular routine. Below are some simple exercises patients can try at home.
Pelvic tilt
Lie on your back with your knees bent. In this relaxed position, Lift your back so your hips are not touching the floor. Tighten your abdominal muscles so that the small of your back presses flat against the floor. Hold for five seconds then relax. Repeat three times and gradually build to 10 repetitions.Knees-to-chest
Lie on your back with both legs straight. Bring one knee up to your chest, pressing the small of your back into the floor (pelvic tilt). Hold for five seconds and repeat five times. Repeat exercise on other leg.Back stretch
Lie on your stomach. Use your arms to push your upper body off the floor. Hold for five seconds. Let your back relax and sag. Repeat 10 times. Discontinue any exercise that produces or increases pain in the leg.Wednesday, October 6, 2010
Pain Management Support & Information
There are many organizations and support groups that are focused on providing both assistance and information on pain management. Chronic pain is complex and all patients require a different treatment plan.There are no easy answers. Get the support you need, from medical physicians and from others who, like yourself, are walking this path.
Here are selected links to those resources:
American Pain Foundation
American Academy of Pain Medicine
American Cancer Society
American Chronic Pain Association
American Pain Society
National Institute of Neurological Disorders and Stroke
http://www.arthritis.org/understanding-pain.php
http://www.painandhealth.org/
Here are selected links to those resources:
American Pain Foundation
American Academy of Pain Medicine
American Cancer Society
American Chronic Pain Association
American Pain Society
National Institute of Neurological Disorders and Stroke
http://www.arthritis.org/understanding-pain.php
http://www.painandhealth.org/
Friday, October 1, 2010
OUR WEBSITE IS READY !
We are so excited that our website is finally finished!
We hope you'll check it out!
Our website provides patients information about our doctors, conditions we treat, procedures we offer and answers to questions they may have.
http://www.austinspineandpain.com/
We hope you'll check it out!
Our website provides patients information about our doctors, conditions we treat, procedures we offer and answers to questions they may have.
http://www.austinspineandpain.com/
Wednesday, September 29, 2010
New Study Reports Ginger Effective for Muscle Pain Relief
GLENVIEW, IL, Sept. 15, 2010 – Daily doses of raw or heat-treated ginger are effective for relieving muscle pain following strenuous exercise, according to research reported in The Journal of Pain, published by the American Pain Society, ampainsoc.org.
Though a favorite remedy of Chinese medicine practitioners for centuries, ginger has not been studied widely as a pain reliever. Some research, however, has shown that ginger may have anti-inflammatory and analgesic properties similar to nonsteroidal anti-inflammatory drugs. In one study, four to 36 weeks of daily ginger doses (30 to 500 mg.) achieved reductions in knee pain from osteoarthritis.
Researchers from the University of Georgia and Georgia College and State University examined the efficacy of multiple days of ginger doses for relieving experimentally induced muscle pain from 18 eccentric muscle exercises. For the study, student volunteers were tested on 11 consecutive days while taking ginger supplements. Seventy-four students were divided in three groups given either raw ginger, heated ginger or placebo. The authors hypothesized that pain ratings after exercise would be lower in the ginger group compared to placebo subjects.
Results from the subjects’ responses data showed that both raw and heat-treated ginger lowered muscle pain intensity after eccentric exercise by 25 and 23 percent, respectively. Heat treating ginger, therefore, did not increase the analgesic benefit.
About the American Pain Society
Based in Glenview, Ill., the American Pain Society (APS) is a multidisciplinary community that brings together a diverse group of scientists, clinicians and other professionals to increase the knowledge of pain and transform public policy and clinical practice to reduce pain-related suffering. APS was founded in 1978 with 510 charter members. From the outset, the group was conceived as a multidisciplinary organization. APS has enjoyed solid growth since its early days and today has approximately 3,200 members. The Board of Directors includes physicians, nurses, psychologists, basic scientists, pharmacists, policy analysts and others
Sunday, September 26, 2010
Two Causes of Pain: Pinched Nerve vs. Disc Pain
By: Peter F. Ullrich, Jr., MD
In identifying the cause of the patient’s pain, there are two general types of spinal disc problems physicians classify as the cause of the pain:
It should be kept in mind that all the terms – herniated disc, pinched nerve, bulging disc, slipped disc, ruptured disc, etc.– refer to radiographic findings seen on a CT scan or MRI scan. While these test results are important, they are not as meaningful as the patient's specific symptoms and the doctor's physical exam results are in determining the source of the back pain and then evaluating potential back care and pain treatments.
In identifying the cause of the patient’s pain, there are two general types of spinal disc problems physicians classify as the cause of the pain:
- Pinched nerve – When a patient has a symptomatic herniated disc, it is not the disc space itself that hurts, but rather the disc herniation is pinching a nerve in the spine. This produces pain that is called radicular pain or radiculopathy (e.g., nerve root pain) leading to pain that may be referred to other parts of the body, such as from the low back down the leg or from the neck down the arm. Leg pain stemming from a pinched nerve in the lower spine is usually described as sciatica.
- Disc pain – When a patient has a symptomatic degenerated disc (one that causes low back pain and/or leg pain), it is the disc space itself that is painful and the source of pain. This type of pain is typically called axial pain.
It should be kept in mind that all the terms – herniated disc, pinched nerve, bulging disc, slipped disc, ruptured disc, etc.– refer to radiographic findings seen on a CT scan or MRI scan. While these test results are important, they are not as meaningful as the patient's specific symptoms and the doctor's physical exam results are in determining the source of the back pain and then evaluating potential back care and pain treatments.
Friday, September 24, 2010
What Treatments Do Pain Medicine (or Pain Management) Specialists Provide?
Pain medicine (or pain management) specialists provide many diverse treatments including activity modification, medication, diagnostic and therapeutic injections, physical therapy, and alternative types of care such as acupuncture, manipulation, and music or art therapy. Multidisciplinary pain medicine combines two or more treatments to maximize pain control. Treatments include:
Some pain patients require stronger medications to manage pain. These medications are technically called Schedule II drugs and require a special type of prescription. Schedule II drugs (like morphine) are carefully regulated. Because of the addiction potential and other risks associated with taking a Schedule II medication, you may be asked to sign a treatment agreement. The agreement puts into writing important information you and your pain management doctor have agreed to. The terms of the agreement may include using one pharmacy for all prescription medications, how to take care not to lose medication, detailed dosing information, and what do to in case side effects develop. In cases where potent narcotics are prescribed, a pain agreement is simply good medicine!
- Restrict activities that increase pain (activity modification)
- Prescription medication: Non-steroidal anti-inflammatory drugs, muscle relaxants, narcotics (opioids), anti-depressants, and anti-seizure drugs. Some anti-depressant and anti-seizure drugs have proven to help manage types of chronic pain.
- Injection therapy: Injections help to pinpoint the cause of pain, as well as provide pain relief. Therapies include epidural steroid, facet joint, and sacroiliac joint injections; and nerve root, medial branch, peripheral and sympathetic nerve blocks.
- Physical Therapy: Heat/ice, massage, spinal traction, transcutaneous electrical nerve stimulation (TENS), ultrasound, and therapeutic exercise.
- Pulsed Radiofrequency Neurotomy is a minimally invasive procedure that prevents nerves from sending pain signals to the brain.
- Rhizotomy uses heated electrodes to turn off pain signals from specific spinal nerves.
- Spinal Cord Stimulation is an implanted device that produces electrical impulses to block pain perception.
- Intrathecal Pumps are sometimes called pain pumps. The device is surgically implanted and dispenses measured doses of medication within the spinal canal.
- Acupuncture is the insertion of very fine, sterile and disposable needles into any of the body's 20 Meridian points or 2,000 acupuncture points. Acupuncture is central to Traditional Chinese Medicine (TCM), which includes other holistic therapies.
- Manipulation is performed by chiropractors, osteopathic doctors (DO), and some physical therapists - although the therapy varies among these professions. Manipulation is the therapeutic application of manual pressure or force to treat a musculoskeletal disorder.
- Music and art therapy are ways to distract your thoughts away from pain. Besides a creative outlet, these therapies promote relaxation, provide a means for emotional expression, help to reduce stress, increases self-esteem, and are fun.
Some pain patients require stronger medications to manage pain. These medications are technically called Schedule II drugs and require a special type of prescription. Schedule II drugs (like morphine) are carefully regulated. Because of the addiction potential and other risks associated with taking a Schedule II medication, you may be asked to sign a treatment agreement. The agreement puts into writing important information you and your pain management doctor have agreed to. The terms of the agreement may include using one pharmacy for all prescription medications, how to take care not to lose medication, detailed dosing information, and what do to in case side effects develop. In cases where potent narcotics are prescribed, a pain agreement is simply good medicine!
Tuesday, September 7, 2010
And so it begins..
We have worked very long and hard trying to get Republic Spine and Pain open.
Its all coming together and this office, which we know with the leadership of our fellowship trained physicians, our loving staff and comfort friendly facility will be offering Austin Texas a wonderful service.
Opening September 2010
Its all coming together and this office, which we know with the leadership of our fellowship trained physicians, our loving staff and comfort friendly facility will be offering Austin Texas a wonderful service.
Opening September 2010
Follow us on twitter.com/treatpainnow
or visit our website
Tuesday, August 17, 2010
What do pain management specialists do?
For thousands of years, doctors have been helping to relieve their patients' pain with a variety of medications and treatments. Like other areas of medicine, a new subset of doctors have become specialists in treating pain. They are focused on managing all types of pain - studying what causes it, how the body reacts to it, how different medications dull or eliminate the pain, and how other treatments can be used to relieve many painful conditions.
The Specialty of Chronic Pain Management
1. What does a pain management specialist do?
A pain management specialist is a physician with special training in evaluation, diagnosis, and treatment of all different types of pain. Pain is actually a wide spectrum of disorders including acute pain, chronic pain and cancer pain and sometimes a combination of these. Pain can also arise for many different reasons such as surgery, injury, nerve damage, and metabolic problems such as diabetes. Occasionally, pain can even be the problem all by itself, without any obvious cause at all.
As the field of medicine learns more about the complexities of pain, it has become more important to have physicians with specialized knowledge and skills to treat these conditions. An in-depth knowledge of the physiology of pain, the ability to evaluate patients with complicated pain problems, understanding of specialized tests for diagnosing painful conditions, appropriate prescribing of medications to varying pain problems, and skills to perform procedures (such as nerve blocks, spinal injections and other interventional techniques) are all part of what a pain management specialist uses to treat pain. In addition, the broad variety of treatments available to treat pain is growing rapidly and with increasing complexity. With an increasing number of new and complex drugs, techniques, and technologies becoming available every year for the treatment of pain, the pain management physician is uniquely trained to use this new knowledge safely and effectively to help his or her patients. Finally, the pain management specialist plays an important role in coordinating additional care such as physical therapy, psychological therapy, and rehabilitation programs in order to offer patients a comprehensive treatment plan with a multidisciplinary approach to the treatment of their pain.
2. What should I look for in a pain management specialist?
The most important consideration in looking for a pain management specialist is to find someone who has the training and experience to help you with your particular pain problem and with whom you feel a comfortable rapport. Since many types of chronic pain may require a complex treatment plan as well as specialized interventional techniques, pain specialists today must have more training than in the past, and you should learn about how your pain physician was trained and whether he or she has board certification in pain management. All our physicians at Republic Spine and Pain completed a pain management fellowship at UT Southwestern at Dallas.
3. How can I be referred to a pain management specialist?
The best way to be referred to a pain management specialist is through your primary care physician. Most pain physicians work closely with their patients' primary care physicians to insure good communication, which in turn helps provide the optimum treatment for their patients. Patients are also often referred by specialists who deal with different types of pain problems. Back surgeons, neurologists, cancer doctors, as well as other specialists usually work regularly with a pain physician and can refer you to one.
Republic Spine and Pain accepts most insurance plans.
4. What should I expect during my first visit to a pain management specialist?
On your first visit to a pain management specialist, he or she will get to know you and begin to evaluate your particular pain problem. This will usually involve a detailed history, a physical exam and review of tests that you have had performed. The questions you are asked and the physical examination will focus on your particular problem, but your pain physician will want to know about past and current medical history as well.
Often you will be given a questionnaire before your first visit that will ask detailed questions about your pain problem, and you will probably be asked to bring any imaging studies (such as X-rays, computed tomography [CAT] scans, or magnetic resonance imaging [MRI] scans) or other tests that have already been done. You should know before your first visit whether or not a procedure is anticipated. If so, you may need a driver to take you home.
Most importantly, this visit is an opportunity for your pain physician to begin to analyze all of this new information and discuss with you an initial assessment of your pain problem. He or she may know exactly what is causing your pain, or perhaps further diagnostic procedures will be needed. But no matter what type of problem you have, you should leave this first visit with a clearer understanding of your pain and the course of further evaluation and treatment that is planned.
The Specialty of Chronic Pain Management
1. What does a pain management specialist do?
A pain management specialist is a physician with special training in evaluation, diagnosis, and treatment of all different types of pain. Pain is actually a wide spectrum of disorders including acute pain, chronic pain and cancer pain and sometimes a combination of these. Pain can also arise for many different reasons such as surgery, injury, nerve damage, and metabolic problems such as diabetes. Occasionally, pain can even be the problem all by itself, without any obvious cause at all.
As the field of medicine learns more about the complexities of pain, it has become more important to have physicians with specialized knowledge and skills to treat these conditions. An in-depth knowledge of the physiology of pain, the ability to evaluate patients with complicated pain problems, understanding of specialized tests for diagnosing painful conditions, appropriate prescribing of medications to varying pain problems, and skills to perform procedures (such as nerve blocks, spinal injections and other interventional techniques) are all part of what a pain management specialist uses to treat pain. In addition, the broad variety of treatments available to treat pain is growing rapidly and with increasing complexity. With an increasing number of new and complex drugs, techniques, and technologies becoming available every year for the treatment of pain, the pain management physician is uniquely trained to use this new knowledge safely and effectively to help his or her patients. Finally, the pain management specialist plays an important role in coordinating additional care such as physical therapy, psychological therapy, and rehabilitation programs in order to offer patients a comprehensive treatment plan with a multidisciplinary approach to the treatment of their pain.
2. What should I look for in a pain management specialist?
The most important consideration in looking for a pain management specialist is to find someone who has the training and experience to help you with your particular pain problem and with whom you feel a comfortable rapport. Since many types of chronic pain may require a complex treatment plan as well as specialized interventional techniques, pain specialists today must have more training than in the past, and you should learn about how your pain physician was trained and whether he or she has board certification in pain management. All our physicians at Republic Spine and Pain completed a pain management fellowship at UT Southwestern at Dallas.
3. How can I be referred to a pain management specialist?
The best way to be referred to a pain management specialist is through your primary care physician. Most pain physicians work closely with their patients' primary care physicians to insure good communication, which in turn helps provide the optimum treatment for their patients. Patients are also often referred by specialists who deal with different types of pain problems. Back surgeons, neurologists, cancer doctors, as well as other specialists usually work regularly with a pain physician and can refer you to one.
Republic Spine and Pain accepts most insurance plans.
4. What should I expect during my first visit to a pain management specialist?
On your first visit to a pain management specialist, he or she will get to know you and begin to evaluate your particular pain problem. This will usually involve a detailed history, a physical exam and review of tests that you have had performed. The questions you are asked and the physical examination will focus on your particular problem, but your pain physician will want to know about past and current medical history as well.
Often you will be given a questionnaire before your first visit that will ask detailed questions about your pain problem, and you will probably be asked to bring any imaging studies (such as X-rays, computed tomography [CAT] scans, or magnetic resonance imaging [MRI] scans) or other tests that have already been done. You should know before your first visit whether or not a procedure is anticipated. If so, you may need a driver to take you home.
Most importantly, this visit is an opportunity for your pain physician to begin to analyze all of this new information and discuss with you an initial assessment of your pain problem. He or she may know exactly what is causing your pain, or perhaps further diagnostic procedures will be needed. But no matter what type of problem you have, you should leave this first visit with a clearer understanding of your pain and the course of further evaluation and treatment that is planned.
Subscribe to:
Posts (Atom)












